Contents [show]
A More Severe Mpox Clade Is on the Rise
Understanding Mpox Clade I: Deadlier and More Infectious
You might recall the global monkeypox outbreak of 2022-2023, but now there’s an even more serious strain on the radar: Mpox Clade I.
Unlike the previous outbreak caused by Mpox Clade II, this strain is spreading swiftly through parts of Africa, with alarming reports of over 18,000 cases this year, including among children.
Tragically, more than 600 deaths have been attributed to this severe variant, prompting the World Health Organization (WHO) to declare it a public health emergency of international concern.
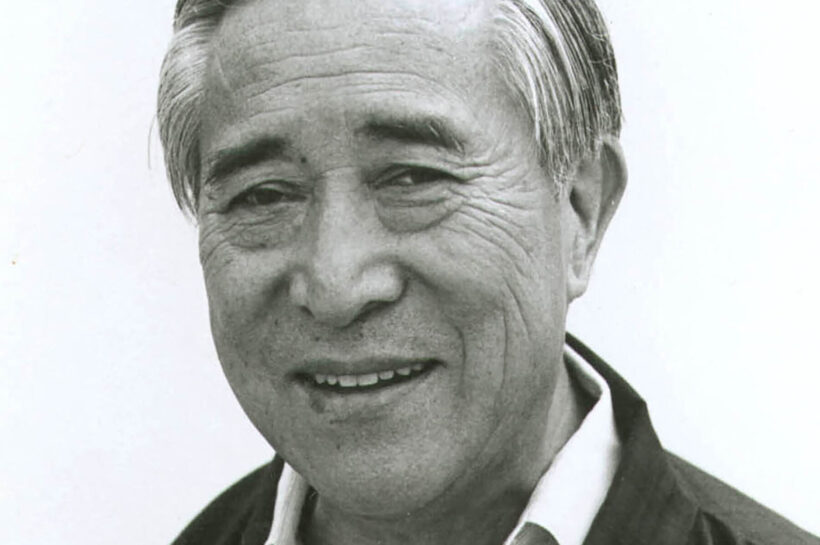
Dean Blumberg, chief of pediatric infectious diseases at UC Davis Children’s Hospital, weighed in to help us better understand this more dangerous strain of the virus and what it means for global health.

What is a Clade, and Why is Mpox Clade I More Dangerous?
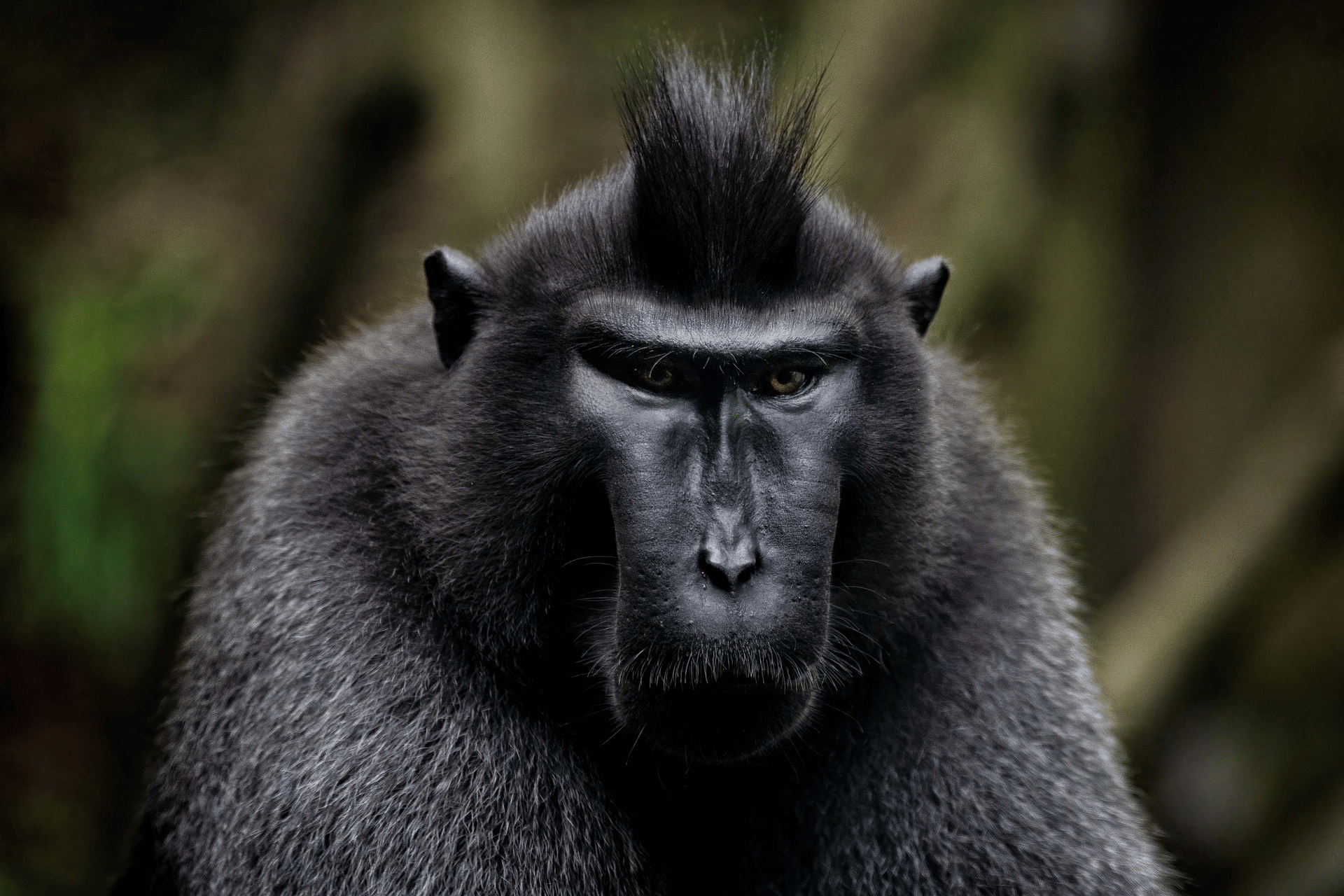
A clade refers to a group of organisms that share a common ancestor. In the case of the mpox virus (previously called monkeypox), WHO has identified two main clades: Mpox Clade I and Mpox Clade II.
While the latter was responsible for the widespread outbreaks in 2022 and 2023, Mpox Clade I is proving to be more deadly and infectious.
What’s particularly concerning is that Clade I is now appearing in countries that have never reported mpox cases before.
As of early September, cases were identified not only in Africa but also in Sweden, Thailand, and Pakistan, likely linked to travel to affected regions in Africa.
Spotting the Symptoms of M-pox Clade I
Familiar Symptoms with a Deadlier Impact
- Rash
- Fever
- Sore throat
- Headache
- Muscle aches
- Back pain
- Swollen lymph nodes
However, what sets Clade I apart is its heightened severity. The rash starts as flat lesions and progresses through blistering, becoming pustules filled with pus, which can be painful and last for weeks.
While symptoms usually resolve within two to four weeks, people with weakened immune systems may face much longer recovery times—and a higher risk of complications.
Transmission and Prevention: How Does M-pox Spread?
M-pox is transmitted primarily through close, personal contact.
This includes direct skin-to-skin interactions, respiratory droplets from talking or breathing close to an infected person, and even contaminated materials like clothing or bedding.
Pregnant individuals can also pass the virus to their unborn child, and in some cases, mpox has been contracted from infected animals.
Is There a Vaccine?
Yes, there is a vaccine. The JYNNEOS vaccine, initially developed to combat both smallpox and mpox, is highly effective when administered promptly after exposure.
The two-dose regimen can significantly reduce the severity of the disease if given within a few days of exposure.
Those who wait longer may still see a reduction in symptoms, but early vaccination remains the best line of defense.
Testing, Treatment, and What to Do if You’re Exposed
Testing for mpox involves a health care provider taking a sample from a lesion and sending it to a lab for confirmation.
While most patients can recover with supportive care and pain management, there are antiviral treatments like Tecovirimat available for those facing severe cases.
If you think you’ve been exposed to mpox, UC Davis infectious disease experts recommend contacting your primary care physician or urgent care clinic, as monkeypox is not typically an emergency.
However, if severe symptoms like difficulty breathing or neurological issues arise, seek immediate medical care.
What Lies Ahead?
While Mpox Clade I is currently circulating most actively in Africa, its recent spread to other regions underscores the importance of vigilance.
Researchers, like those at UC Davis, are closely monitoring the situation. As we’ve learned from past outbreaks, early awareness and swift response are key to limiting the global impact of this more dangerous strain.
For more information, consult the Centers for Disease Control and Prevention (CDC) or reach out to healthcare providers who can offer guidance on vaccines, testing, and treatment options.
Stay informed, stay cautious, and most importantly, stay safe.
This was 1st reported from: UC Davis.
What Does the CDC Say About Monkeypox (Mpox/M-Pox)?
As concerns about monkeypox, or mpox, continue to grow, it’s important to stay informed about the disease and the available preventive measures. The Centers for Disease Control and Prevention (CDC) has provided detailed guidance on the virus and its vaccine.
Understanding Mpox and the JYNNEOS Vaccine
Mpox is caused by a virus closely related to the smallpox virus. To combat this, the JYNNEOS vaccine was developed as a two-dose regimen that protects against both mpox and smallpox. For optimal protection, it’s essential to receive both doses of the vaccine, with the second dose administered four weeks after the first. If you’ve missed the recommended window, it’s crucial to get the second dose as soon as possible to maintain your immunity.
Vaccination is a key tool in stopping the spread of mpox. However, even after receiving the vaccine, individuals are advised to avoid close, skin-to-skin contact with anyone diagnosed with mpox.
Risk of Reinfection and Vaccine Recommendations
While it is possible for someone who has recovered from mpox to contract the virus again, the CDC reports that reinfection is extremely rare, occurring in less than 0.1% of previously infected individuals. Additionally, reinfections tend to be milder than the initial illness. As a result, those who have already had mpox are not currently recommended to receive the JYNNEOS vaccine.
The CDC recommends the vaccine for people at higher risk, including those who:
- Had known or suspected exposure to someone with mpox
- Had a sex partner recently diagnosed with mpox
- Are gay, bisexual, or men who have sex with men, or are transgender, nonbinary, or gender-diverse, with certain risk factors such as:
- A recent diagnosis of a sexually transmitted disease (e.g., chlamydia, gonorrhea, or syphilis)
- Multiple sex partners
- Sexual activity in commercial venues or at large events where mpox transmission is occurring
Vaccination Details and Side Effects
The JYNNEOS vaccine can be administered either subcutaneously (under the skin) or intradermally (between the top layers of the skin). Both methods are effective, and individuals can discuss the best option with their healthcare provider. Side effects, which may include pain, redness, and itching at the injection site, are common but not severe.
It’s important to note that while protection begins after the first dose, full immunity develops two weeks after the second dose.
For more information on vaccination locations and options, contact your local health department or visit CDC‘s website.